To view information on another disease, click on SOD and Pancreatitis Library.!
..


..
..
Distal Pancreatectomy
The term distal pancreatectomy describes resection of variable amounts of the body and tail of the pancreas. Partial pancreatic resection is recommended for patients with diffuse (moderate to severe) parenchyma disease without ductal dilation, especially in the tail and body. Local resection of major pancreatic sites of involvement may be sufficient for those patients with regional disease, whereas a 95% distal resection is recommended for patients with diffuse disease. Ninety-five percent distal pancreatectomy entails removal of the spleen and almost all of the pancreas, except for a thin rim of tissue within the "C" loop of the duodenum. Splenic preservation is attempted, but often fails because dissection of splenic vessels from the chronically inflamed and scarred pancreas is extremely difficult. This procedure provides pain relief for 75–80% of patients and has a mortality rate less than 5%.
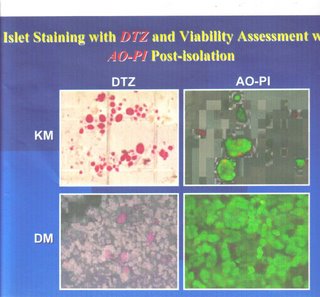
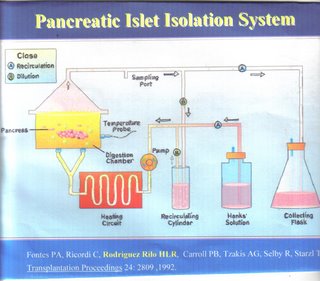
Total Pancreatectomy: Removal of the entire pancreas is utilized on occasion to treat chronic pancreatitis when other treatments are unsuccessful. This operation has no additional complication rate compared to the Whipple procedure. Removal of all the insulin-producing cells of the entire pancreas may cause a form of diabetes that is difficult to manage. Some hospitals and surgeons offer total pancreatectomy combined with transplantation of the patient's own insulin-producing cells, (Auto Islet Transplantation) in order to keep the patients from becoming diabetic. (TP/ICT)
 ..
..